2019/08/14(水)
Special lecture 「Design-driven approach to drug discovery and translational research」
Rieko Yajima Ph.D,
[Profile]
 |
Stanford University, Director of Drug Discovery Innovation, SPARK Program in Translational Research, School of Medicine |
[Summary]
Today, I will be specifically talking about the work we do at the Stanford SPARK Program - we are a translational research program that takes early-stage discoveries from research labs on our campus and our mission is to train our faculty and students on how to move the research forward so that it will be attractive to investors or bio-pharma companies to develop into therapeutics that will reach patients.
So, we're here at a life sciences conference, so I know you are all aware that developing new medicines is very difficult. In the United States, the average timeline from discovery of a new biological target to getting a therapeutic approved to use in humans is 12-15. The pathway for drug discovery and development is often described as a pipeline (going here from left to right) with universities conducting the bulk of the basic and preclinical research. This is the engine for finding new ways to treat diseases (what's referred to here as Discovery) and then moving to the middle where industry - biotech and pharma companies - will take those discoveries and test them to see if they work in humans in clinical trials. Finally, if you're lucky, the company will file for regulatory approval and manufacture the drug which then gets prescribed to patients. Each of these phases requires high levels of expertise and multiple disciplines - not just scientific but also in intellectual property, business development, regulatory affairs, patient care and user experience. No one is an expert in all areas; effective collaboration is a must.
In addition to time, to make things worse, this is a very expensive process, costing up to $1B depending on how you count. Most striking for me, however, is the high failure rate of drug discovery. About 1 in 10 drugs that enter clinical trials receives regulatory approval in the United States. That's a success rate of a little over 10%. Think about that - can you imagine spending $100s of millions of dollars on a product that you are developing and it only has about 10% chance of success. So, we all need to do better.
Today I'm going to focus on the translational research part of the pipeline. So that we have a shared definition here - it's the gap between academic research, where promising scientific discoveries are made, and industry research, where companies can take these discoveries and see if they will work in humans and if so, to manufacture the drug for patients to use.
You might be wondering why the system is so inefficient and costly. And there are many reasons for failure along the pipeline. That's a whole another lecture. But the point that I want to make is that most failures in drug development occur late in the process - during Phase 2 and Phase 3 clinical trials, after hundreds of millions of dollars are already spent. For example, the success rate of moving from Phase 2 to Phase 3 clinical trials in the United States is 25%. As an industry, this number has not improved in the past decade. When you look at the reason for failures in Phase 2 clinical trials, you find that 20% fail due to lack of safety (so they are too toxic to be used), while 50% fail due to lack of efficacy (lack of efficacy means that the drug doesn't work for the health problem or indication it is intended to treat). Again, drug development is unique in this regard and different from other industries in that drugs will fail to get approval due to scientific failure rather than market failure or technical failure.
At SPARK, we look broadly at the following question: How might we improve the science upstream of clinical research so that it may reduce failures late in the drug development pipeline? So the rest of my presentation will focus on what we are doing to address the translation gap between academia and industry.
So let's look at the roles of academia and industry a bit more closely. The word pipeline is not quite accurate to describe drug development, because it sounds like as long as we do great research at our universities, then industry is eager to take the ideas and move them forward.
You would think that translation would be the easy part.
In principal, our overarching goal is the same - we all want new therapies that can benefit patients.
In reality, however, it's important to look at the incentive structures that drive these two sectors. Because it's these incentive structures that drive what actually occurs in practice and contributes to the inefficiency of drug development.
For instance, here are some of the considerations that affect what type of research gets done in academia versus industry and why the two often don't meet at the translational center.
First, the research context: in academia we tend to focus on basic biological research. Here, we intentionally reduce complexity in order to ask a very specific, often very narrow question. In contrast, humans are complex - and when you provide a treatment it can affect them as a whole, not just the biological pathway that was investigated. There are also many factors, including ones that are not in your control, that can determine whether a clinical trial will be successful for not. So clinical research tends to have more uncertainties that have to be accounted for.
In academia, we are rewarded for novelty and new discoveries - finding a new phenomena that has never been proven scientifically before. This means that for academics, there is little incentive in the system to shift research aims so that it is more conducive for drug development. In contrast, the research goals for industry are largely set by the regulatory agencies - drug companies must do the research that shows that a drug is safe and that it works (that it's efficacious).
I'll just note that the risks that are felt by each side also play a role - in industry, they have financial pressures to not make mistakes. While in academia, there is more tolerance for taking risks and having failure - not too much failure though, otherwise no one will want to fund you or trust your work.
So if you compare what academia values with what industry values, you will see that both sides have different standards for evidence and expectations for what is quality data. The point here is that one is not better than the other - they are simply different. And because they are different, this leads to a lot of mistrust between scientists at universities and scientists in industry.
And this leads to assumptions and biases. Industry researchers believe that academic research is not high enough quality to translate (for ex, there are surveys published in Nature that show this opinion and there is some evidence that reproducibility in some fields of academic research is a legitimate concern). Meanwhile, academic researchers believe that as long as their paper is published in Science, Nature or Cell, that industry will knock of the door and want to translate.
Both are not entirely true but they are common assumptions.
As a result, most academic discoveries are not translated because these projects never make it out of the university. And because academics are not trained in translational science (to do the work of applied science of drug discovery), the success rates are often quite low.
It's clear that if you want to improve translation coming out of any university, in other words, moving ideas out of universities and developed to benefit patients, a system is needed that overcomes these two economic systems, because the incentives structures are misaligned.
And this should matter to all of us as citizens, whether you are in drug discovery or not, because most research done at universities is funded by taxpayer dollars and is intended to have societal benfits.
So SPARK was started 13 years ago by a professor at Stanford, who wanted to address these issues. Professor Daria Mochly-Rosen is a biochemistry faculty member and she had one of these experiences that I just mentioned. Published a compelling research paper that she thought would be an important target for treating myocardial damage due to heart attack, and she expected that it would be fairly straight forward to translate and develop a treatment for patients. It turns out that no company was interested in her science. So she started a company with her graduate student. She met with over 50 venture capitalists and no one was interested. Huge shock. To make a long story short, through a lot of persistence, it took over 10 years, but the treatment that she developed, based on the discovery made in her research lab, was successful in getting regulatory approval. During those ten years, her startup company was acquired by Amgen, a large biotech company, the indication was changed from cardiovascular disease, and there were many twists and turns along the way. Given everything she learned from scientists and other experts in industry, she realized that most academics have no training in how to do this and will likely encounter the same problems she did.
So that's the original idea behind SPARK. I should add that a number of features about the SPARK program include practices that are commonly used in design practices and we continue to expand and test the ways that design practices might improve scientific research in drug discovery.
SPARK is a group of researchers at Stanford who want to move their discoveries into the clinic to treat patients, and we partner with volunteer experts from drug development companies that provide wisdom and strategic advice. It's important to note that this is a self-selected group of people -from both sides - academic and industry - that are collaborating outside of their own incentive structures.
For industry advisors, they are representing themselves as individuals - not the interests of their companies - and are volunteering their time and expertise so that the projects - any of our projects - have the best chance of success at helping patients.
For academics, there is little incentive in the system to change practices to make their research more conducive for drug development. In academia, particularly at Stanford, publishing is still king - if you want to cure cancer, that's great - but you will still need to publish your research at a high level, even if you start your own company. So we look for researchers that are really committed to translation, because it does take additional effort to see these projects through to the end.
So, at SPARK, we do 3 things:
- Train Stanford faculty, students and post-docs on how to do translational research
- Fund projects to de-risk the science and advance the research
- Provide mentorship from industry advisors and connect project teams to other expertise
and research facilities on campus (this latter part is more like an accelerator)
We are fortunate to draw on industry experts from across the bay area. These experts come from all fields: medicinal chemistry, cell and molecular biology, pharmacology, regulation, intellectual property, and the investment community. The one thing they all have in common is experience and perspective downstream of academia to help inform academics what they don't know.
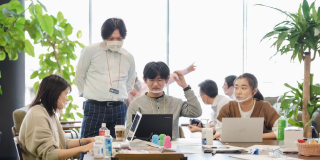
Our experience with the SPARK program has shown that face- to-face collaborative work can remove the negative biases that divide academic and industry communities, so that they can develop trust.
We meet in person once a week throughout the whole year - and this part is important. We meet in person to develop trust and mutual respect between academia and industry.
During these meetings, we accomplish two goals of the program.
1) We're educating translational scientists - our lectures cover all aspects of drug discovery and development - -from target validation and toxicology (biology) to regulatory, intellectual property and pitching to VCs and starting your company.
2) We have our SPARK teams present their research updates to get feedback on research strategy and results from our advisors.
I want to say a few more things about the culture of SPARK at Stanford. And this was by design, from the Directors of SPARK, Daria Mochly Rosen and Kevin Grimes.
Prior to joining the SPARK team last year, I spent two and half years as a Research Scholar at the Center for Design Research at Stanford. One of the key points that I took away was that Design is about intentionality. Understanding where you are in the present (in this case understanding the context of industry versus academia) and being clear about where you would like to go.
The format of these meetings is designed to promote open discussion and mutual respect.
So, how do you design for that? For starters, that means no hierarchy - students and Nobel laureates can question the science. High-risk ideas are encouraged - including ideas that are unlikely to be pursued in industry. We want these ideas to have a chance. Again, the economic system within academia is not tied to financial returns or quarterly reports. We should allow for this, whereas industry has financial pressures that make this not so easy. If we can de-risk these projects enough, then industry can pick them up when they are ready for further development.
We are also not looking for consensus amongst our advisors -- we are not looking for agreement. Instead, we want our project teams to hear many options and ideas to consider before deciding on the right strategy to move forward (in design this is often called idea generation - you expand your idea space before you select one to prototype or test).
We also have our project teams begin their work with SPARK by thinking through their project by Starting with the end in mind. Drug discovery is complex - there is often not a single right answer but choices you make with tradeoffs that are good and bad. So we have them think through a variation on something called need-finding. In this case, the questions are like: What type of clinical endpoints are you striving for? How does this inform your preclinical studies? Who will pay for the drug? What delivery mechanism is best for the patient? What's the IP landscape - do you have freedom to pursue this idea further? This is often a deal killer. These are the issues that project teams attempt to address up front, in addition to the science.
It's worth to point out these cultural practices that I describe - they don't come easy and it's something you build over time. It's something we continue to strive for and improve. And this starts with our leaders who model this behavior for us.
Let me turn to the outcomes and try to show you some evidence on how this works in practice.
In SPARK, we give a modest amount of funding - $50K per year for up to 2 years. From there, the SPARK teams will try to advance their projects until there is an opportunity to develop it further in the private sector - either through licensing with an existing bio-pharma company or by creating a start up company. '
I should note that commercialization or return on investment is not our metric for success. We also take in projects that don't have a commercial upside (including infectious disease that primarily affect the developing world or sometimes rare diseases). For these projects, the goal is to bring the projects into the clinic through an investigator initiated clinical trial, and to see if we can change medical treatment practice.
So we have several dozen ongoing projects, and over a hundred that have completed or graduated from the SPARK program. Out of those, about half end up being commercialized, resulting in 30 startup companies, and 25 being advanced to clinical trial. The rest of the projects fail either due to proof of concept or if someone on the team leaves and the project stalls.
At SPARK, project ideas can come from anyone: students, post-docs, professors; biologists, chemists, clinicians, engineers.
The SPARK model has been expanded to over 60 universities around the world. Each SPARK program is adapted to their location, strengths and local ecosystem. As it should.
For example, at Stanford, we focus only on therapeutics and some diagnostics (biomarkers).
Whereas for other SPARK sites, they work primarily on devise.
When I look at SPARK, I see many design practices and principals that are native to how the SPARK program got started. I think of Professor Daria Mochly Rosen as a natural design thinker, especially in the way that SPARK guides its projects and the way our community works. Our newest efforts expand and test additional design principals and practices further upstream of translational research into the discovery of new targets. This includes introducing the human context at the very start of the drug discovery process and how to embrace human complexity as a way to complement reductionist science. One of the approaches we are using involves cell-wide measurements at multiple scales - DNA, RNA, protein - these "multi-omics" methods can help us understand the human context, if you will, as we figure out the right treatment for the right person. This has always been the huge promise or holy grail of personalized medicine.
We are still early in our efforts here but this is the direction we are moving towards. One of the indications we are working on is schizophrenia - a complex mental disorder (complex genetics, variety of risk factors and a condition with symptom heterogeneity).
In conclusion, I'd like to emphasize that at SPARK, we think of ourselves as a community. It really takes a group effort - and for us, it's not just a group of academics; it's truly an academic-industry partnership. The end result is that we've selected projects with strong science, we've had industry advisors guide and vet the research along the way, and we track projects based on milestones that move the science down the translation path. And we think all of these factors make a difference in getting to a successful outcome.